
Radiating pain, a form of discomfort that spreads from a specific point in the body along a particular nerve pathway, is a common yet often misunderstood symptom. It refers to pain perceived at a location different from its source, typically suggesting an issue with nerve function or signaling (1). It is often confused with referred pain, which is pain felt in a location different from the source of the pain. The crucial distinction between these two types of pain lies in their distinct pathways: while radiating pain typically follows a direct nerve pathway, referred pain is less predictable.
Understanding radiating pain is essential for accurate medical diagnostics and effective patient care. It can provide vital clues about the underlying health conditions that cause it, from simple muscle strain to more serious issues like nerve damage or disease. For example, pain radiating down the arm might be indicative of a cardiac issue, whereas pain radiating down the leg could suggest a problem with the lower back or hips (2). Hence, medical practitioners and patients alike can greatly benefit from a comprehensive understanding of radiating pain.
Defining Radiating Pain
Radiating pain is a type of pain that spreads from the point of origin to other areas of the body. This is in contrast to localized pain, which is confined to a specific area where an injury or illness is present. Radiating pain often occurs along a nerve pathway and can be described as sharp, burning, or electric-like in nature (3).
Patients experiencing radiating pain often describe it as pain that moves or travels from one area to another. For example, a patient with sciatica (a common condition associated with radiating pain) might describe pain that starts in the lower back and moves down the leg, following the path of the sciatic nerve (4).
The exact nature of radiating pain can vary widely based on its cause. Understanding the unique characteristics of this type of pain – its pattern, associated symptoms, and exacerbating or relieving factors – is crucial in guiding further diagnostic evaluations and treatment plans (5).
Causes of Radiating Pain
Radiating pain can be caused by numerous medical conditions, typically related to nerve irritation, inflammation, or damage. Depending on the specific nerve or group of nerves affected, radiating pain can present in different areas of the body. Here are several conditions known to cause radiating pain:
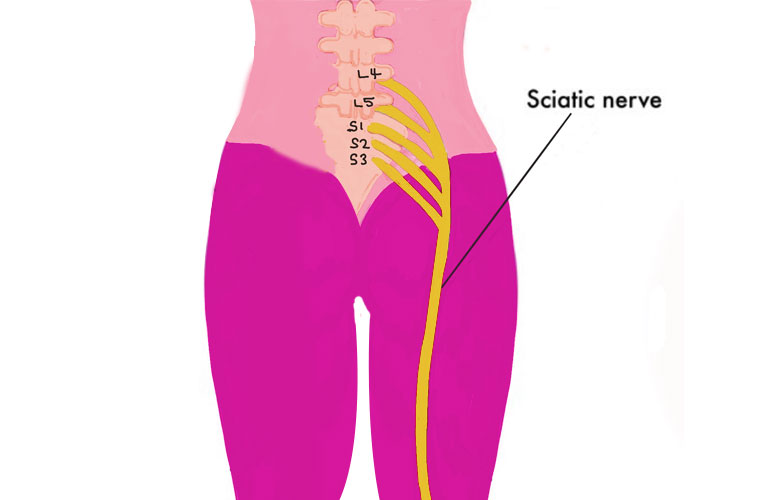
Sciatica: Sciatica is often a result of a herniated disc or bone spur in the lumbar spine that irritates or compresses part of the sciatic nerve. The sciatic nerve is the longest nerve in the body, running from the lower back, down the back of each leg to the foot. As such, irritation or compression can cause radiating pain to extend from the lower back through the buttocks and down the leg, commonly affecting only one side of the body. Typically, this results in pain radiating from the lower back down into the leg, often on one side (6).

Herniated Disc: In this condition, one of the cushioning discs between the vertebrae in the spine ruptures, which can press on the nerves. The pain typically radiates along the pathway of the nerve that’s being compressed. For instance, a herniated disc in the lower back could cause radiating leg pain (sciatica), while one in the neck might cause radiating arm pain (7).

Cardiac Conditions: Certain heart conditions, like angina or myocardial infarction (heart attack), can result in radiating pain. The discomfort typically starts in the chest and can radiate to other areas like the left arm, shoulder, neck, jaw, or back. In some cases, pain might be felt only in these radiating locations and not in the chest. This is due to the heart muscle not getting enough oxygen because of a blocked coronary artery (8).
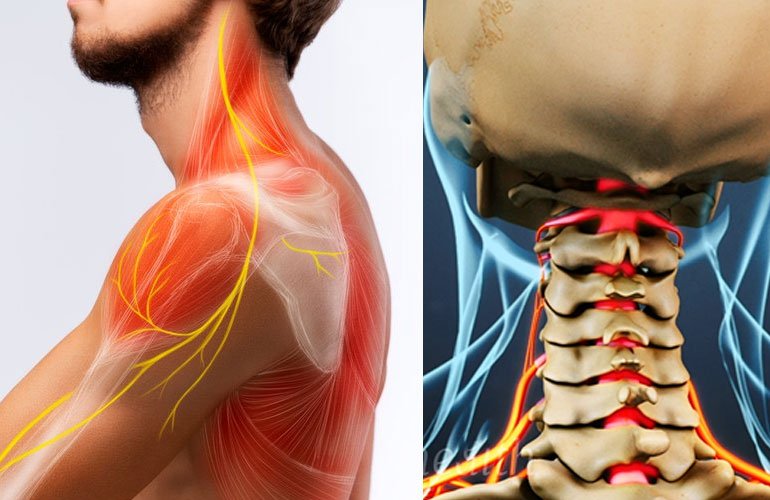
Cervical Radiculopathy: When a nerve in the neck becomes inflamed or compressed, the condition—also known as a pinched nerve—occurs. The origin is often a herniated disc or bone spur in the neck region of the spine. The pain associated with cervical radiculopathy typically radiates down the path of the afflicted nerve into the arm and hand, sometimes leading to symptoms such as numbness or weakness in the arm.

Peripheral Neuropathy: Peripheral neuropathy results from damage to the peripheral nerves, which spread out from the brain and spinal cord to the rest of the body (9). Conditions such as diabetes or autoimmune diseases often cause it. Depending on which nerves are affected, peripheral
neuropathy can cause radiating pain in different areas of the body, often described as a burning, tingling, or prickly sensation. For instance, if it affects the legs’ nerves, the pain could radiate from the thigh down to the foot.

Gallstones: In some cases, abdominal conditions like gallstones can cause radiating pain. A gallstone blocking the gallbladder can cause intense pain in the upper right abdomen or the center of the abdomen. This pain can radiate to the right shoulder or back.
Each of these conditions can lead to radiating pain due to their impact on specific nerves or nerve pathways. Irritation, inflammation, or damage to these nerves can cause pain signals to be sent along the length of the nerve, resulting in pain that is felt at a distance from the originating source.
Diagnosis of Radiating Pain
Diagnosing the causes of radiating pain requires a multi-pronged approach that relies heavily on the patient’s reported symptoms, a comprehensive medical history, physical examinations, and a variety of diagnostic tests. Due to the complex nature of radiating pain, it often presents significant challenges to healthcare providers.
1. Patient History and Physical Examination:
The first step in diagnosing radiating pain is a thorough patient interview and physical examination. The healthcare provider will ask detailed questions about the pain, such as its location, nature (sharp, dull, burning), intensity, duration, and any factors that may exacerbate or relieve it. The specific location, nature, and timing of the pain can provide clues about its cause (10). They will also inquire about any other accompanying symptoms, as well as the patient’s personal and family medical history. A physical examination will then be conducted, focusing on the nervous system and musculoskeletal system, to identify any signs of nerve irritation or damage, muscle weakness, or other abnormalities that could be causing the pain.
2. Diagnostic Tests and Procedures:
Depending on the results of the patient interview and physical examination, several diagnostic tests might be conducted to further pinpoint the source of the pain.
Imaging tests such as X-rays, MRIs, and CT scans can provide detailed images of the body’s structures, helping to identify conditions such as herniated discs, bone spurs, or tumors that might be pressing on a nerve (11).
Electromyography (EMG) and nerve conduction studies (NCS): These tests can assess the electrical activity in muscles and the speed of nerve signal conduction, respectively. They can help diagnose conditions that involve nerve damage or irritation (12).
However, diagnosing radiating pain can be complex due to its potentially multifactorial nature. Some patients may have more than one condition contributing to their pain, and in some cases, an exact cause may not be identifiable despite extensive evaluation (13).
3. Challenges and Complexities in Diagnosing Radiating Pain:
Diagnosing radiating pain can be particularly challenging due to its complex nature. The pain is often felt far from its actual source, which can make it difficult to identify the underlying cause. For example, someone with a herniated disc in their lower back may feel pain radiating down their leg due to the compression of the sciatic nerve – a condition known as sciatica.
Furthermore, many conditions can cause similar symptoms, which can complicate the diagnostic process. For instance, both a herniated disc and spinal stenosis can cause radiating leg pain, but they require different treatment approaches. In some cases, a person may have more than one condition contributing to their pain, which can further complicate diagnosis and treatment.
Despite these challenges, advancements in medical technology and a better understanding of the mechanisms of pain have greatly improved the ability to diagnose and treat radiating pain. However, due to its complex nature, managing radiating pain often requires a multidisciplinary approach that may involve physicians, physical therapists, and other healthcare providers.
Read More: Self-diagnosis of lumbar intervertebral disc prolapse/PLID/Disc Herniation
Treatment Options for Radiating Pain
Managing radiating pain involves a comprehensive approach that combines medical interventions with lifestyle adjustments and self-care strategies. The goal is to treat the underlying cause, manage the pain, and improve quality of life.
1. Medical Interventions:
Several medical interventions are available, including medication, physical therapy, and in some cases, surgery.
Medication: Over-the-counter pain relievers like NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) and acetaminophen are often the first line of treatment. For more severe pain, physicians might prescribe opioids, though they are generally used for short-term relief due to their potential for dependence and addiction (14). Steroid injections can also help reduce inflammation around the nerve and relieve pain. Antidepressants and anticonvulsants have also proven effective in managing certain types of nerve pain.
Physical Therapy: Physical therapists can design personalized exercise programs that help strengthen muscles, improve flexibility, and promote optimal posture, all of which can help alleviate radiating pain. A study in the Archives of Physical Medicine and Rehabilitation found significant improvements in radiating leg pain in patients who underwent a physical therapy regimen for sciatica (15).
Interventional Treatments: For certain causes of radiating pain, specific interventional treatments may be beneficial. These can include epidural steroid injections for sciatica, nerve blocks, and radiofrequency ablation, which uses heat to interrupt pain signals from specific nerves (16).
Surgery: When other treatments are ineffective, surgery might be an option. This is often the case for conditions like herniated discs or spinal stenosis, where relieving pressure on the affected nerve can significantly reduce pain (17). For instance, procedures such as lumbar discectomy and spinal decompression surgery can relieve pressure on the nerves and subsequently alleviate pain.
2. Self-Care Strategies and Lifestyle Adjustments:
Self-care and lifestyle adjustments can also significantly contribute to managing radiating pain.
- Exercise and Physical Activity: Regular exercise not only strengthens the body but also boosts endorphin production, which can naturally help reduce pain.
- Healthy Diet: A balanced diet can help maintain optimal weight, which reduces strain on the spine and joints, thus alleviating some types of radiating pain.
- Heat and Cold Therapy: Applying heat or cold to the affected area can help reduce inflammation and alleviate pain.
- Stress Management Techniques: Stress can exacerbate pain. Practices such as yoga, mindfulness, and meditation can help manage stress levels and improve pain management.
3. Analysis of Benefits and Potential Side Effects:
While these treatment options can significantly improve the quality of life of those suffering from radiating pain, each comes with potential benefits and drawbacks. Medication, while often effective for pain relief, can have side effects such as gastrointestinal problems, dependency issues, and more. Physical therapy is generally a safe option, but it requires commitment and patience, as benefits are often seen over time. Surgery, although it can be highly effective, comes with risks such as infection and complications from anesthesia.
Ultimately, the treatment plan for radiating pain should be individualized, taking into account the patient’s specific condition, overall health, pain severity, and lifestyle. It’s crucial that patients work closely with their healthcare providers to choose the most appropriate treatment strategy and adjust it as needed.
Read More: The best treatment of PLID/ Disc herniation / Disc prolapse in Bangladesh
Patient Experience and Management
Radiating pain, regardless of its underlying cause, can significantly impact a patient’s quality of life. It can affect daily functioning, disrupt sleep, and may even lead to psychological consequences such as depression and anxiety. Therefore, managing and living with radiating pain involves addressing both the physical and emotional aspects of the condition. A study published in Pain Medicine found that patients with lumbar radiculopathy, a common cause of radiating pain, reported significantly lower quality of life scores compared to the general population (18).
Strategies for coping with radiating pain often include:
- Understanding the Condition: Gaining knowledge about the condition and its treatment options can give patients a sense of control and help them make informed decisions about their care.
- Adherence to Treatment: Compliance with prescribed treatments, whether it’s medication, physical therapy exercises, or lifestyle changes, is crucial for managing pain and preventing it from worsening.
- Activity Modification: Patients may need to avoid activities that exacerbate pain and gradually reintroduce activities as their condition improves (19).
- Pain Tracking: Keeping a pain diary can help patients and healthcare providers understand the patterns of pain, identify triggers, and evaluate the effectiveness of treatments.
- Psychological Support: Given the impact on mental health, psychological support can be crucial. This could include cognitive-behavioral therapy to help patients develop coping strategies for dealing with chronic pain (20).
- Healthy Lifestyle: A balanced diet, regular exercise, adequate sleep, and avoidance of alcohol and tobacco can all contribute to overall well-being and help in managing pain.
Conclusion
Radiating pain is a complex condition that requires a comprehensive and individualized approach to diagnosis and treatment. Despite the challenges, understanding the causes of radiating pain and the available treatment options can significantly enhance the patient’s quality of life.
However, it’s important for anyone experiencing radiating pain to seek professional medical advice. Self-diagnosis and treatment can be risky, and only a qualified healthcare provider can accurately diagnose the cause of the pain and propose an appropriate treatment plan.
The field of pain management continues to evolve, and future research holds the promise of more effective treatment strategies for radiating pain. Continued exploration in this area can lead to better patient outcomes and improved quality of life for those living with radiating pain.
FAQ’s
What is radiating pain?
Radiating pain is a type of pain that spreads from the source of the pain to other areas of the body. This is often due to irritation or injury to nerves or spinal structures, causing the pain to travel along nerve pathways.
What are the common causes of radiating pain?
Common causes of radiating pain include herniated discs, sciatica, spinal stenosis, pinched nerves, and certain injuries or conditions that affect the spinal cord or nerves.
How is radiating pain diagnosed?
The diagnosis of radiating pain begins with a comprehensive medical history and physical examination. Healthcare providers often use diagnostic tests such as X-rays, MRI scans, CT scans, and nerve conduction studies to identify the underlying cause of the pain.
What are the treatment options for radiating pain?
Treatment options for radiating pain vary depending on the underlying cause. They can include medications, physical therapy, interventional procedures like nerve blocks or injections, and in some cases, surgery. Lifestyle changes, such as regular exercise, maintaining a healthy weight, and managing stress, can also help manage the symptoms.
How does radiating pain impact quality of life?
Radiating pain can significantly impact a person’s quality of life. It can restrict mobility, interfere with daily activities, and contribute to mental health issues such as anxiety and depression. Effective management strategies can help individuals cope with the impact of radiating pain on their lives.
Is radiating pain a sign of a serious condition?
While radiating pain can be uncomfortable, it’s not always a sign of a serious condition. However, in some cases, it may indicate a significant issue such as a herniated disc or spinal stenosis. It’s essential to consult a healthcare provider to accurately diagnose and treat the underlying cause of radiating pain.
Can radiating pain go away on its own?
In some cases, radiating pain may resolve on its own, especially if it’s due to a temporary inflammation or irritation of a nerve. However, chronic or persistent radiating pain requires medical attention to identify and treat the underlying cause.
How can I manage radiating pain at home?
Home management strategies for radiating pain include rest, applying heat or cold to the affected area, over-the-counter pain relievers, and gentle stretching exercises. However, these strategies should complement, not replace, professional medical advice and treatment.
Reference
1. Koes, B.W., Van Tulder, M. and Thomas, S., 2006. Diagnosis and treatment of low back pain. Bmj, 332(7555), pp.1430-1434. https://www.bmj.com/content/332/7555/1430.short
2. Klabunde, R., 2011. Cardiovascular physiology concepts. Lippincott Williams & Wilkins.
https://books.google.com/books?hl=en&lr=&id=27ExgvGnOagC&oi=fnd&pg=PP2&dq=2.%09Klabunde,+R.+E.+(2012).+Cardiovascular+Physiology+Concepts.+Lippincott+Williams+%26+Wilkins.&ots=_jeA8ei3eA&sig=0NtV2PJYhMhX5EKWnijuS_PULrQ
3. Bogduk, N., 2009. On the definitions and physiology of back pain, referred pain, and radicular pain. PAIN®, 147(1-3), pp.17-19. https://www.sciencedirect.com/science/article/pii/S0304395909004576/pdf?md5=4b26276053a7251c45fd23862bffa673&pid=1-s2.0-S0304395909004576-main.pdf&_valck=1
4. Jensen, R.K., Kongsted, A., Kjaer, P. and Koes, B., 2019. Diagnosis and treatment of sciatica. bmj, 367.
https://www.bmj.com/content/367/bmj.l6273.full
5. Loeser, J.D. and Treede, R.D., 2008. The Kyoto protocol of IASP basic pain terminology. PAIN®, 137(3), pp.473-477.
https://www.sciencedirect.com/science/article/pii/S0304395908002327/pdf?md5=2aa8358133ec8948ca62f10f67484b68&pid=1-s2.0-S0304395908002327-main.pdf&_valck=1
6. Valat, J.P., Genevay, S., Marty, M., Rozenberg, S. and Koes, B., 2010. Sciatica. Best practice & research Clinical rheumatology, 24(2), pp.241-252.
https://www.sciencedirect.com/science/article/pii/S1521694209001417
7. Koes, B.W., Van Tulder, M.W. and Peul, W.C., 2007. Diagnosis and treatment of sciatica. Bmj, 334(7607), pp.1313-1317.
https://www.bmj.com/content/334/7607/1313?flh=
8. McSweeney, J.C., Cleves, M.A., Zhao, W., Lefler, L.L. and Yang, S., 2010. Cluster analysis of women’s prodromal and acute myocardial infarction symptoms by race and other characteristics. The Journal of cardiovascular nursing, 25(4), p.311.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2884391/
9. Callaghan, B.C., Cheng, H.T., Stables, C.L., Smith, A.L. and Feldman, E.L., 2012. Diabetic neuropathy: clinical manifestations and current treatments. The lancet NEUROLOGY, 11(6), pp.521-534
https://www.sciencedirect.com/science/article/pii/S1474442212700650
10. Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001 Feb 1;344(5):363-70. doi: 10.1056/NEJM200102013440508. PMID: 11172169. https://www.nejm.org/doi/10.1056/NEJM200102013440508?url_ver=Z39.88 2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
11. Chou, R., Qaseem, A., Snow, V., Casey, D., Cross Jr, J.T., Shekelle, P., Owens, D.K. and Clinical Efficacy Assessment Subcommittee of the American College of Physicians and the American College of Physicians/American Pain Society Low Back Pain Guidelines Panel*, 2007. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Annals of internal medicine, 147(7), pp.478-491.
https://www.acpjournals.org/doi/abs/10.7326/0003-4819-147-7-200710020-00006
12. Kimura, J., 2013. Electrodiagnosis in diseases of nerve and muscle: principles and practice.
13. Stochkendahl, M.J., Kjaer, P., Hartvigsen, J., Kongsted, A., Aaboe, J., Andersen, M., Andersen, M.Ø., Fournier, G., Højgaard, B., Jensen, M.B. and Jensen, L.D., 2018. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. European Spine Journal, 27, pp.60-75. https://link.springer.com/article/10.1007/s00586-017-5099-2
14. Chou, R., Gordon, D.B., de Leon-Casasola, O.A., Rosenberg, J.M., Bickler, S., Brennan, T., Carter, T., Cassidy, C.L., Chittenden, E.H., Degenhardt, E. and Griffith, S., 2016. Management of Postoperative Pain: a clinical practice guideline from the American pain society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. The journal of pain, 17(2), pp.131-157. https://www.sciencedirect.com/science/article/pii/S1526590015009955
15. Albert, H.B. and Manniche, C., 2012. The efficacy of systematic active conservative treatment for patients with severe sciatica: a single-blind, randomized, clinical, controlled trial.
https://journals.lww.com/spinejournal/FullText/2012/04010/The_Efficacy_of_Systematic_Active_Conservative.2.aspx
16. Manchikanti, L., Abdi, S., Atluri, S., Benyamin, R.M., Boswell, M.V., Buenaventura, R.M., Bryce, D.A., Burks, P.A., Caraway, D.L., Calodney, A.K. and Cash, K.A., 2013. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain physician, 16(2S), p.S49.
https://search.proquest.com/openview/df36eed0fe918c15a14afa2f15f5fb69/1?pq-origsite=gscholar&cbl=5453642
17. Weinstein, J.N., Tosteson, T.D., Lurie, J.D., Tosteson, A.N., Hanscom, B., Skinner, J.S., Abdu, W.A., Hilibrand, A.S., Boden, S.D. and Deyo, R.A., 2006. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. Jama, 296(20), pp.2441-2450.
https://jamanetwork.com/journals/jama/article-abstract/204281
18. Hirsch, O., Strauch, K., Held, H., Redaelli, M., Chenot, J.F., Leonhardt, C., Keller, S., Baum, E., Pfingsten, M., Hildebrandt, J. and Basler, H.D., 2014. Low back pain patient subgroups in primary care: pain characteristics, psychosocial determinants, and health care utilization. The Clinical Journal of Pain, 30(12), pp.1023-1032.
https://journals.lww.com/clinicalpain/fulltext/2014/12000/Low_Back_Pain_Patient_Subgroups_in_Primary_Care_.2.aspx
19. Liddle, S.D., Baxter, G.D. and Gracey, J.H., 2004. Exercise and chronic low back pain: what works?. Pain, 107(1-2), pp.176-190. https://www.sciencedirect.com/science/article/pii/S0304395903004342
20. Veehof, M.M., Oskam, M.J., Schreurs, K.M. and Bohlmeijer, E.T., 2011. Acceptance-based interventions for the treatment of chronic pain: a systematic review and meta-analysis. Pain®, 152(3), pp.533-542.
https://www.sciencedirect.com/science/article/pii/S0304395910006871





